Imagine being able to detect breast cancer before it even begins, a concept that once seemed impossible but is now becoming a clinical reality thanks to the incredible advancements of artificial intelligence. Recent research, including a study published in JAMA Network Open, reveals that AI technology can predict the development of breast cancer up to five years earlier than traditional screening methods can detect it, a breakthrough that is not just impressive but potentially life-saving.

So how does AI achieve this remarkable feat, and what does it mean for the future of early detection, diagnosis, and personalized care? Artificial intelligence is transforming healthcare, particularly in the realm of early disease detection, and in the case of breast cancer, AI systems have been trained to recognize warning signs long before they evolve into detectable tumors. These systems, powered by deep learning algorithms, analyze thousands or even millions of mammograms, but they don’t merely search for obvious anomalies; they dig deeper, identifying subtle changes in breast tissue, slight texture variations, and tiny microcalcifications that even the most skilled radiologists might miss.
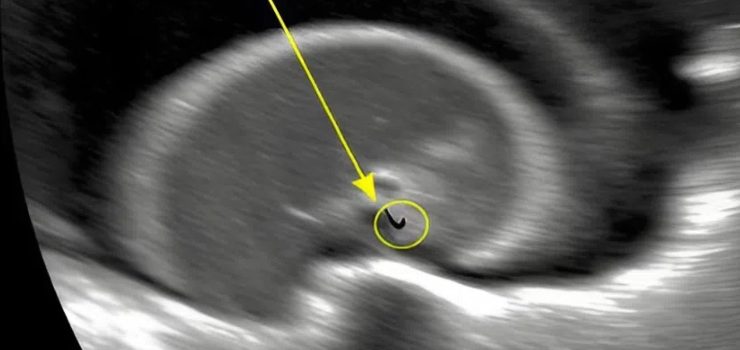
These subtle indicators are not random; they are often the earliest hints that cancer could be developing, even if the patient feels perfectly healthy. Some AI models have demonstrated the ability to flag high-risk cases as many as four to six years before clinical symptoms would appear. Deep learning, a specialized branch of machine learning, operates by mimicking the brain’s own method of processing information, utilizing layers of artificial neurons that analyze medical images piece by piece. When the AI scans a mammogram, it meticulously examines features like tissue density, shape, and structure, comparing what it observes against vast databases of known outcomes before generating a risk score estimating how likely it is that a patient might develop cancer in the future.
With each image it analyzes, the AI continues to learn and refine its accuracy, making it an increasingly powerful tool for diagnosis. Some fear that AI might replace doctors, but in reality, it is designed to support and enhance their work, not replace them. Radiologists often face the daunting task of reviewing thousands of scans, most of which show no abnormalities, and with AI serving as a “second reader,” radiologists can concentrate more effectively on the scans that truly demand attention. A recent study in Radiology showed that AI assistance reduced radiologists’ workloads by almost 40 percent without sacrificing diagnostic accuracy, leading to faster screenings, quicker diagnoses, and ultimately better outcomes for patients.
There are several clear advantages to integrating AI into breast cancer detection. Unlike humans, AI doesn’t suffer from fatigue and can detect minute details that human eyes might overlook. It prioritizes urgent cases, speeding up the diagnostic process so treatment can begin sooner for those who need it most. It also reduces false positives, sparing patients the emotional distress and medical risks associated with unnecessary biopsies. Furthermore, AI’s ability to generate risk scores enables doctors to create customized follow-up plans, recommending more frequent screenings for high-risk individuals while sparing low-risk patients from unnecessary tests. Since AI can compare mammograms over time, it is particularly adept at spotting slow, creeping changes that signal early-stage cancer development. For patients, this new technology provides a level of reassurance and empowerment never seen before; a routine mammogram no longer just delivers a clean or unclear result but now can provide a detailed, scientifically backed risk assessment. Those identified as high-risk can take proactive steps such as lifestyle changes, closer monitoring, or even preventative treatments, while low-risk patients can avoid the costs and stress of excessive screening. Looking forward, AI’s role in breast cancer care will expand far beyond mammograms. As electronic health records grow more sophisticated, AI could integrate data from blood tests, genetic profiles, and lifestyle factors to offer full-body risk assessments and truly personalized healthcare. However, with all this promise comes responsibility. AI must be carefully monitored to avoid biases, particularly since datasets used for training must represent diverse populations. Privacy remains a significant concern too, and AI systems must adhere to strict data protection standards to keep patient information safe. But with careful oversight and continuous improvement, the benefits of AI far outweigh its challenges. Artificial intelligence is ushering in a new era in the battle against breast cancer, detecting warning signs invisible to the human eye and giving doctors and patients a critical advantage—time. This isn’t some far-off future dream; it’s happening right now, and as technology continues to advance, we are moving toward a future where cancer might be stopped before it ever truly begins.